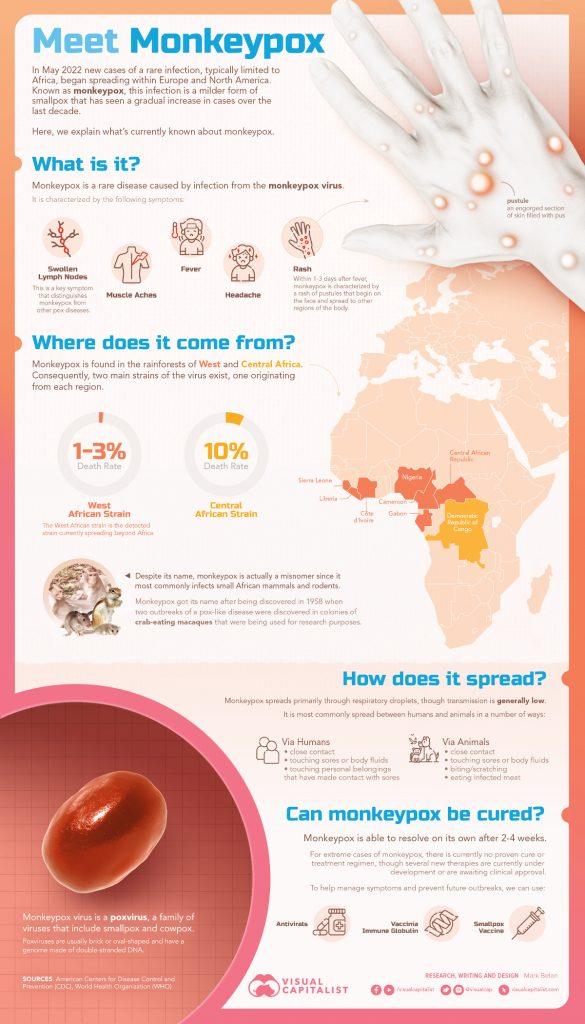
What is monkeypox?

Monkeypox disease is caused by the monkeypox virus, which belongs to a member of the Orthopoxvirus genus in the family Poxviridae. Immunity plays a vital role in such infections.
Monkeypox is a viral zoonosis which is a virus transmitted to humans from animals with symptoms same to those seen in the past in smallpox patients, even though it is clinically less severe.
How does it spread?
Transmission of Monkeypox virus from one person to another through close contact with lesions, respiratory droplets, body fluids and contaminated materials such as bedding.
History
In 1958, Monkeypox was first found. Also, at that time two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, from that the name ‘monkeypox’ was given. The first human case of monkeypox was identified in 1970 in the Democratic Republic of Congo during a period of intensified effort to abolish smallpox. After that, monkeypox has been reported in humans in other central and western African countries.
Signs & Symptoms
Usually, the incubation period of monkeypox is 6 to 13 days but can range from 5 to 21 days. There is an incubation period (After infection) which lasts on average 7-14 days.
Initial symptoms like fever, malaise, headache, weakness, etc. marks the beginning of the prodromal period.
A characteristic that distinguishes infection of monkeypox from smallpox is the growth of swollen lymph nodes (lymphadenopathy). Swelling of the lymph nodes may be generalized which means involving many different locations on the body or localized to several areas like the neck and armpit.
A rash appears, shortly after the prodrome. Typically Lesions started to develop simultaneously and evolve together on any given part of the body. The development of lesions progresses through four stages—macular, papular, and vesicular, to pustular—before scabbing over and resolving.
Key Characteristics for Identifying Monkeypox
According to CDC, Lesions are
- well-circumscribed,
- deep-seated, and
- often develop umbilication, which means resemble a dot on the top of the lesion.
Before rashes fever is observed. Lymphadenopathy is a common symptom. The disseminated rash is centrifugal (more lesions on extremities, face). Lesions on palms, and soles are also observed. Lesions are described as painful until the healing phase when they become itchy (crusts).
The progress of monkeypox rash
Generally, the first lesions will be inside the mouth or on the tongue (Enanthem). When a person becomes contagious, this is the first sign of rash marks.
These flat-based lesions (Macules) typically started from the face before spreading across the body, to the arms and legs, then the hands and feet within 24 hours. This stage lasts for one to two days.
Generally, by day three, the rash lesions will become slightly raised and feel firm (Papules). This stage duration is also one to two days.
On the fourth or fifth day, the raised lesions fill up with clear fluid and this stage also lasts for one to two days (Vesicles).
During the sixth to the seventh day, lesions have become pustular which means the lesions become filled with opaque, yellowish fluid and also become sharply raised, firm-feeling, and often round (Pustules). Pustules will even develop a dot on top. This stage is last for about five to seven days before they start to crust over.
From day 14, the lesions will become crusty scabs and at this stage, the lesions, which patients describe as painful throughout the stages when will become itchy (Scabs). After all the lesions fall off, the person is considered non-contagious.
In about 95% of cases the lesions occur on the face; in 75% of cases the lesions observed on the palms of the hands and soles of the feet; the lesion skin inside the mouth in 70% of cases reported and lesions on the genitals in 30% of cases and in the eyes in 20% of cases reported.
WHO
Monkeypox in pregnancy
Information about monkeypox infection among pregnant women is very restricted, as most prior descriptions of monkeypox outbreaks in Africa do not report a description of the natural history of outbreaks among pregnant women.
In Zaire, one probable case of perinatal infection has been found. At approximately 24 weeks gestation, a pregnant woman developed a febrile sickness with a rash, and later, the monkeypox virus was isolated from a vesicular lesion. Six weeks later she delivered a 1500 g infant who had a generalized skin rash which is look like monkeypox.
This may reflect declining immunity in all communities due to the cessation of smallpox vaccination. Transmission can also occur via the placenta from mother to fetus (which can lead to congenital monkeypox) or during close contact during and after birth. While close physical contact is a well-known risk factor for transmission, it is unclear at this time if monkeypox can be transmitted specifically through sexual transmission routes. Studies are needed to better understand this risk.
Prevention
Raising awareness of risk factors and educating the people about the measures they can take to reduce exposure to the virus is the main prevention strategy for monkeypox.

How can it be controlled?
In recent times, the case fatality ratio has been approximately 3–6%. The transmission of Monkeypox disease is to humans, by close contact with an infected person or animal, or with material contaminated with the virus. Also, severe cases can occur.
GOOD NEWS: The symptoms of monkeypox are lasts for 2 to 4 weeks. No need to worry as usually, it is a self-limited disease.
Vaccination
Vaccination against smallpox was demonstrated via several observational studies to be approximately 85% effective in preventing monkeypox. In recent times, the original (first-generation) smallpox vaccines are no longer available to the general public.
A still newer vaccine based on a modified attenuated vaccinia virus (Ankara strain) was accepted for the prevention of monkeypox in 2019. This is a two-dose vaccine for which availability remains limited. Smallpox and monkeypox vaccines are prepared in formulations based on the vaccinia virus because of cross-protection afforded for the immune response to orthopoxviruses.