The vaginal environment plays an important role in health and diseases in reproductive-age women. The vaginal environment is dynamic depending on internal and external factors such as hormone fluctuations, phases of the menstrual cycle, drug treatments such as antibiotics and contraceptives, concomitant pathologies, and habits.
These factors can influence the fragile balance (between good bacteria and pathogens) of the vaginal environment. The source of the pathogens can be both external (environment, sexual partner. . .) or internal, the gastrointestinal tract is one reservoir of opportunistic pathogens able to colonize the vagina.

Bacterial infections like bacterial vaginitis and vaginosis, whose origin lies in the uncontrolled proliferation of pathogenic bacteria. Majorly, all vaginitis and vaginosis treatments have solely been focused on attacking the disproportionately developed bacteria but have not addressed the restoration of a vaginal acidic environment, i.e. the environment allowing the proliferation of lactic acid-producing Bacillus acidophilus (Good bacteria).
It is well known that the risk of Sexually Transmitter Infections is increased in the presence of vaginal infection.
Birth control pills and vaginal health
Another study concludes that levels of estrogen increase during menarche (first menstrual cycle) which leads to an increase in new lactobacilli proliferation and since contraceptives affect the levels of these hormones, they will definitely affect Lactobacillus bacteria. In return will increase the opportunistic pathogens in the vagina and cervix.
The use of the intrauterine contraceptive devices (copper-T) and Oral Contraceptive Pill (birth control pills) changes the normal vaginal bacterial flora, with cervical corrosion and vaginal infections with IUCD users.
The increase in the observed cases of vaginitis infection, especially for IUCD users due to a decrease in Lactobacillus bacteria.
Lactic acid
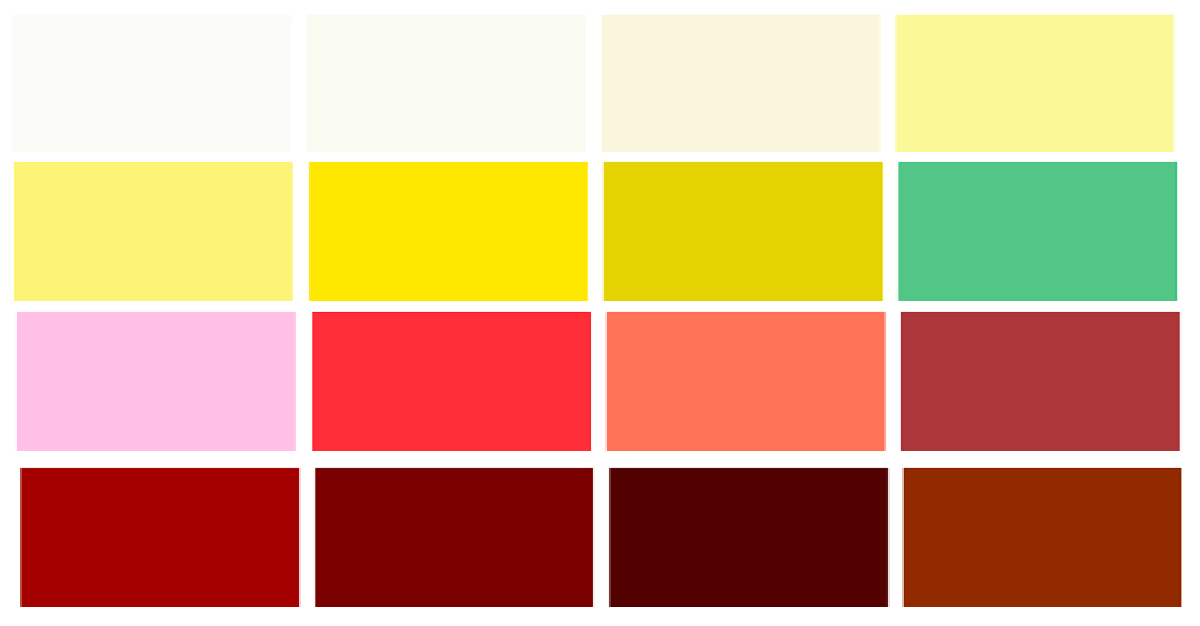
Women worldwide engage in vaginal hygiene practices. The most common active ingredients are antiseptic compounds and lactic acid. A healthy vaginal environment is characterized by an abundance of Lactobacilli (Lactobacillus species produce lactic acid and acidify the vagina (pH < 4.5) ) and creates a hostile environment for most pathogens.
The vaginal protection system is based on the maintenance of a 3.5 to 4.5 acidic pH (highly acidic) where the common and potentially pathogens cannot survive, whereas Lactobacillus are in their ideal environment.
Women are at greater risk of sexually transmissible infections and, in turn, problems with their reproductive health if their vagina doesn’t have high amounts of lactic acid, according to a recent review published in the journal Research in Microbiology. A loss of Lactobacilli and an overgrowth of other anaerobes is indicative of bacterial vaginosis/ infection and is associated with an increased risk of HIV acquisition and transmission, and preterm birth.
The origin of bacterial infections like vaginitis and vaginosis lies in the change of the number of Lactobacilli and/or the alkalization of the vaginal pH, allowing the proliferation of common vaginal pathogenic bacteria and produce symptoms.

Treatment of Vaginal Infection
- Polish Society of Gynecologists and Obstetricians recommendation on the use of antiseptics for treatment of inflammatory vaginitis
- Polyhexamethylene biguanide has no inhibitory effects on Lactobacillus spp. growth.
- Dequalinium chloride: Good efficacy in the treatment of bacterial vaginosis.
- Silver ions: A broad spectrum of anti-inflammatory properties including antifungal activity.
- Boric acid: Maintenance therapy of especially fungal vaginosis and recurrent infections.
- Chlorhexidine: Element of prevention and supportive therapy before and after gynecological surgical procedures
- The treatment of bacterial infection (vaginitis and vaginosis) should be done with the reduction in the number of causing-symptoms pathogens, and also with the primary objective to recover the vaginal pH. It will restore the virtuous circle that maintains a healthy vagina.
- The application of lactic acid, which acidifies the medium, hinders the growth of vaginal pathogens and promotes the proliferation of lactic acid-producing Lactobacilli.
- Use traditional medicines for the pathogens that cause vaginal symptoms in addition to the use of lactic acid afterward, at least for a week, to ensure the normal vaginal ecosystem recovery.
- Another study recommends the use of oral probiotics rather than local administration certainly led to increased compliance and early antipathogenic action of the probiotic into the intestine, which is known to be one of the potential sources of vaginal infection. Once in the vagina, the probiotic may also exert its benefits locally
It’s better to consult the doctor for any such infections, as the treatment differs from patient to patient.
Image Credits: Pexels